What Are Pelvic Floor Disorders?
Understanding Pelvic Floor Disorders
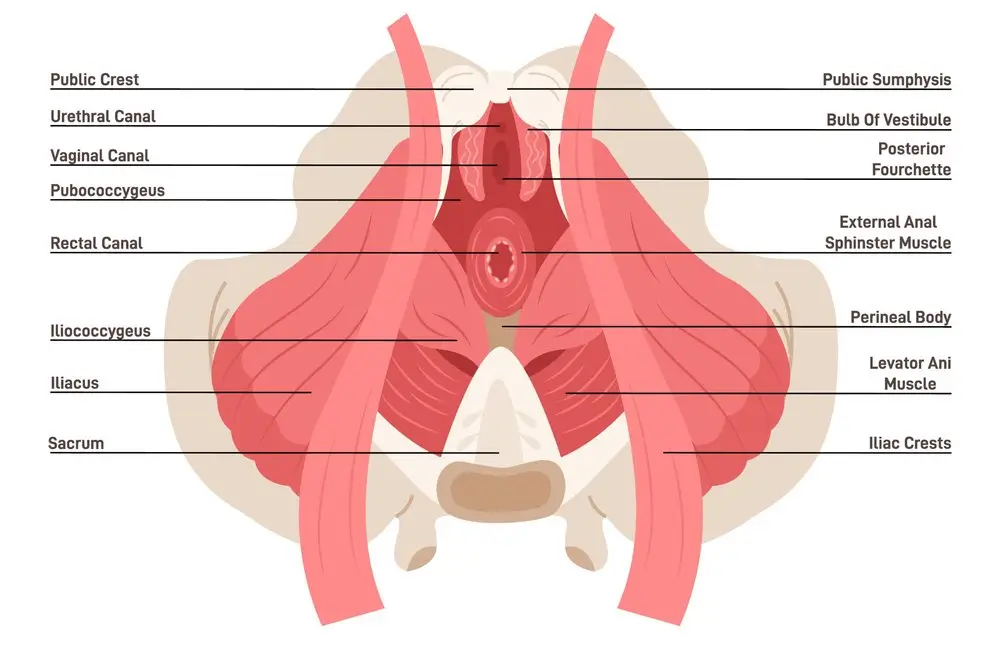
Pelvic floor disorders occur when the muscles, ligaments, and nerves supporting the bladder, uterus, vagina, and rectum become weakened or damaged. This can result from childbirth, chronic conditions, repeated heavy lifting, or surgery, leading to discomfort and loss of function.
At WomanWoRX, we combine expertise from the Urogynecology Center of Minnesota with specialized Pelvic Floor Physical Therapy to provide effective, non-surgical treatment. If pelvic floor issues are affecting your daily life, we’re here to help you regain strength, comfort, and confidence.
Symptoms of Pelvic Floor Disorders
Urinary incontinence:
Loss of bladder or bowel control with leakage of urine or feces
Prolapse:
Descent of pelvic organs; a bulge and/or pressure; “dropped” uterus, bladder, vagina or rectum (Includes Cystocele, Enterocele, Rectocele, Uterine prolapse, Vaginal vault prolapse)
Emptying disorders:
Difficulty urinating or moving bowels
Pelvic pain:
Discomfort to the lower back, pelvis or bladder and/or urethra
Overactive Bladder:
Frequent need to void, bladder pressure, urgency, urge incontinence (difficulty holding back urine when having the urge to urinate)
Fistulas:
Abnormal hole between the vagina and rectum (recto-vaginal), vagina and urethra (urethrovaginal), or vagina and the bladder (vesicovaginal)
Comprehensive Treatments for Pelvic Floor Disorders
Our Foundation
At our foundation practice, Minnesota Women’s Care, we always begin with the least invasive solution. When possible, we choose non-surgical options to help our patients find relief.
One of our most important treatment options is available at WomanWoRX. With a thoughtful combination of Pelvic Floor Physical Therapy, Chiropractic Care, and Exercise, many women can diminish symptoms of pelvic floor disorders and learn how to prevent them in the future.
If your condition requires a different non-surgical option, we’ll refer you to our pelvic floor specialists in the Urogynecology Center.
Other Options
When the non-surgical approach isn’t the right choice, we will refer you to our Urogynecology Center for further diagnostics. Our team can determine what is causing your pelvic floor disorder and provide the most effective options for you.
When surgery is necessary, the Urogynecology Center uses the least invasive procedure to encourage rapid healing and minimize surgical pain. These procedures include:
- Surgical Mesh
- Prolapse Repair
- InterStim
- Axonics
The Advantages of Physical Therapy, Chiropractic Care, and Exercise
Physical therapy (PT) combined with exercise can have a significant impact on pelvic pain. The combination of targeted physical therapy interventions and exercise can help improve pelvic muscle function, reduce pain, and enhance overall quality of life.
Research supporting the effectiveness of PT combined with exercise for pelvic pain is growing. While individual studies may vary, several systematic reviews and meta-analyses have shown positive outcomes in terms of pain reduction, improved function, and quality of life for individuals with various forms of pelvic pain.
Here are some key points regarding the impact of PT combined with exercise on pelvic pain:
Individualized Assessment and Treatment: Physical therapists who specialize in pelvic health can perform a comprehensive evaluation to identify the underlying causes and contributing factors of pelvic pain. This may include assessing muscle imbalances, joint mobility, nerve involvement, and pelvic floor function. Based on the assessment findings, the physical therapist can develop an individualized treatment plan to address the specific needs of the individual.
Pelvic Floor Muscle Rehabilitation: Physical therapy for pelvic pain often involves pelvic floor muscle rehabilitation. This may include exercises to strengthen weak muscles, relax overactive muscles, and improve coordination and control of the pelvic floor. These exercises can be performed under the guidance of a physical therapist who can provide proper technique and progression.
Manual Therapy Techniques: Physical therapists may use various manual therapy techniques to address musculoskeletal issues associated with pelvic pain. This can include techniques such as soft tissue mobilization, myofascial release, joint mobilization, and nerve mobilization. Manual therapy can help alleviate muscle tension, improve joint mobility, and reduce pain.
Education and Self-Management Strategies: Physical therapists play a crucial role in educating individuals about their condition and providing self-management strategies. This may include guidance on posture, body mechanics, bladder and bowel habits, relaxation techniques, and lifestyle modifications to help manage and prevent pelvic pain episodes.
Exercise Prescription: In addition to pelvic floor muscle exercises, physical therapists may prescribe specific exercises to address overall strength, flexibility, and stability. These exercises can target the core muscles, hips, and surrounding areas to improve posture, support the pelvis, and reduce strain on the pelvic region.
Psychological Support: Pelvic pain can have a significant impact on an individual’s emotional well-being. Physical therapists who specialize in pelvic health can provide psychological support and help individuals develop coping strategies to manage the emotional aspects of pelvic pain.
